Coming to terms with being unable to conceive naturally can be stressful, and can leave you feeling angry, depressed and anxious. It can also put additional stress on relationships, intimacy, and your connection with relatives and friends. The impact can be profound and long lasting.
The process of going through IVF (in vitro fertilisation) for months and even years can take its toll as you may experience hopes and disappointments, while managing the implications on your emotions, your body, your relationship and your finances.
Fertility problems affect between 10 per cent and 15 per cent of the population, according to the World Health Foundation. In the UK, one in six couples are affected and the number seeking medical help to start a family has risen dramatically, with more turning to IVF.
But mental health issues rooted in fertility problems are unlikely to end with a clinical intervention to help create a family. The incidence of depression in couples presenting for fertility treatment is significantly higher than in the general population and poor mental health can itself become an obstacle to a successful outcome through IVF.
IVF providers are beginning to give greater priority to the emotional support that is available to couples going through treatment
Although the stigma of mental health remains, IVF providers are beginning to give greater priority to the emotional support that is available to couples going through treatment.
Aileen Feeney, chief executive of the charity Fertility Network UK, says women and men who are unable to start a family suffer from stigma, and are likely to suffer from anxiety and stress.
“Society still largely assumes that you will go on to have a family, sooner or later, and so much of what we do revolves around family life,” she says. “But it doesn’t always work out that way and many people find they cannot conceive naturally. Yet, it can be extremely difficult to come to terms with this, and society gives you constant reminders.”
 A major survey by Fertility Network UK in 2016 revealed that the emotional and social impact of fertility problems was greater than previously recognised. The survey, conducted in association with Middlesex University London, assessed the impact of failing to conceive and the subsequent impact of fertility treatment on both women and men. Some 90 per cent of respondents reported feeling depressed and 42 per cent experienced suicidal feelings.
A major survey by Fertility Network UK in 2016 revealed that the emotional and social impact of fertility problems was greater than previously recognised. The survey, conducted in association with Middlesex University London, assessed the impact of failing to conceive and the subsequent impact of fertility treatment on both women and men. Some 90 per cent of respondents reported feeling depressed and 42 per cent experienced suicidal feelings.
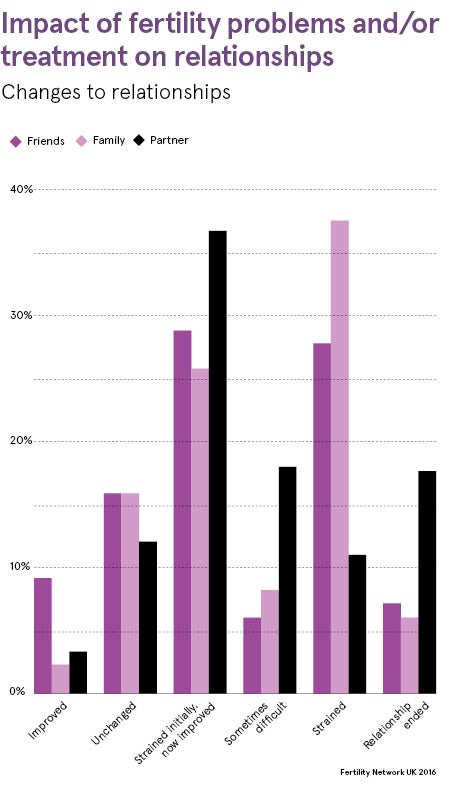
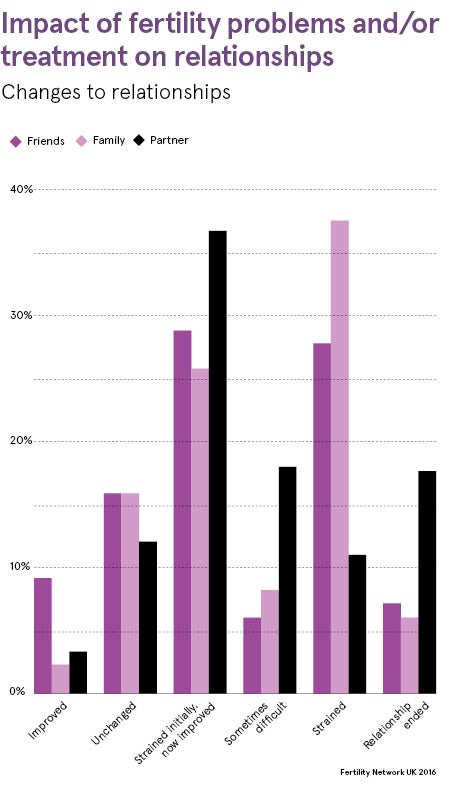
Those who had unsuccessful treatment reported greater distress as well as more frequent suicidal thoughts. More than two thirds of respondents (70 per cent) reported some detrimental impact on the relationship with their partner, while 15 per cent said their relationship ended or was strained as a result of the impact of fertility problems and treatment.
The majority of respondents would have liked to have had counselling if it was free; fewer than half (44 per cent) did have counselling and of these more than half had to pay for some or all of this psychological help. More than half of all respondents reported a lack of local peer support services.
Professor Adam Balen, chair of the British Fertility Society, says: “The survey showed the true picture of living with fertility problems for many people. It can be an incredibly distressing time, and undergoing treatment and facing costs can place a huge amount of stress and pressure on couples and their families.”
The National Institute for Health and Care Excellence recommends that counselling should be offered before, during and after IVF treatment, regardless of the outcome. Counselling should be offered by someone not directly involved in the management of a couple’s fertility problems. This can help couples to understand the implications of treatment and offer support at a critical time, such as when an IVF cycle has been unsuccessful.
In the UK, the Human Fertilisation and Embryology Authority (HFEA) is responsible for the regulation of clinics providing IVF treatment. All clinics licensed by the HFEA must offer couples an opportunity to talk to a counsellor before treatment begins. This helps them to think about their treatment in advance, and how it might affect them and those close to them, in the short term and in the future.
Some clinics offer free counselling, but others charge. Couples researching clinics are advised to ask about this, and whether clinics offer support groups or the opportunity to meet other patients who are undergoing similar treatment.
In addition to the counselling couples may receive from their clinic, the HFEA advises couples to consider seeking counselling on the NHS or privately. This provides an opportunity to explore feelings around fertility more generally and can be done individually or as a couple. GPs provide a gateway to NHS counselling.
For private counselling, the British Infertility Counselling Association has a directory of accredited therapists, with options including telephone and Skype counselling. The HFEA website also lists other support organisations, including the Donor Conception Network and Fertility Friends.
More than half of men would not be open to discussing fertility with their partner
Research shows that more than half of men would not be open to discussing fertility with their partner, yet they are just as at risk of experiencing feelings of sadness, shame, anger, depression or inadequacy. Sadly, there are fewer dedicated support options for men than there are for women. One option is the Men’s Health Forum, which has information about men’s health as well as an online community where men can chat anonymously.
Many support groups welcome individuals and couples so this could be a good place to meet other men with similar experiences, either alone or with a partner. Some men also find it easier to speak to a counsellor who has experience working with men with fertility problems, and can be a trusted and impartial “outsider”.
Getting news that you are not pregnant after a round of IVF treatment can be devastating. Experts advise that it is important to take the time to come to terms with this outcome and give your body and mind time to recover. When you’re ready, talk to your doctor about whether you should try again and what the chance of conceiving might be if you did. Health professionals may suggest a different treatment or discuss any other options for maximising your chances of conceiving. It is also important to consider the financial implications of your decision.
If you’re unable to have more treatment, or you’re not sure if you want to go through treatment again, you may find it helpful to talk your feelings through with a counsellor. Some couples have different opinions on whether to continue with treatment; talking to an impartial professional may help you to think through the issues together and come to an agreement about how to move forward.
IVF treatment continues to make great progress, with new techniques and products bringing real hope to more couples who are unable to conceive naturally. But while pushing these boundaries, the IVF industry must also accept its responsibility to support its clients’ emotional wellbeing as well as their fertility problems.