High-support mental health rehabilitation has been much discussed recently with a new report highlighting the issue of how long patients remain in these facilities, raising important questions for the sector.
Certainly high-support mental health rehabilitation is one of the most challenging areas of healthcare, but it is only by reviewing the role it plays in treating patients with very complex mental health problems and seeking to address the issues raised that the industry will be able to improve outcomes for patients continually and effectively.
For patients who require more intensive care, high-support mental health rehabilitation can be the best solution. Secure mental health services provide crucial treatment and rehabilitation for people who are trying to recover while detained under the Mental Health Act. They may be exhibiting dangerous and challenging behaviour, and may also be a risk to others.
High-support mental health rehabilitation services work with people with very complex needs that cannot always be met by general adult mental
health services.
Cygnet Health Care has been providing a national network of high-quality, specialised mental health services for more than 20 years in partnership with the NHS and local authorities. Our services support people with complex and acute mental health illnesses, including schizophrenia, bi-polar affective disorder, personality disorders, eating disorders, learning disabilities, acquired brain injuries, children’s services and autistic spectrum disorders.
As one of the best quality providers in mental health hospital rehabilitation in the country, our focus is always on the best outcomes for those who use or commission our services.
Patients admitted to high-support rehabilitation hospitals tend to have extensive comorbidities and typically find it hard to sustain significant clinical gains following discharge. A significant proportion of these people have been so-called “revolving-door” patients undergoing repeated readmission to acute wards at the highest cost to the taxpayer. Research from the University of York last year found that 50 per cent of mental health NHS patients experience relapses resulting in admission to hospital, while NHS patients at a Cygnet hospital benefit from a low 29 per cent relapse rate.
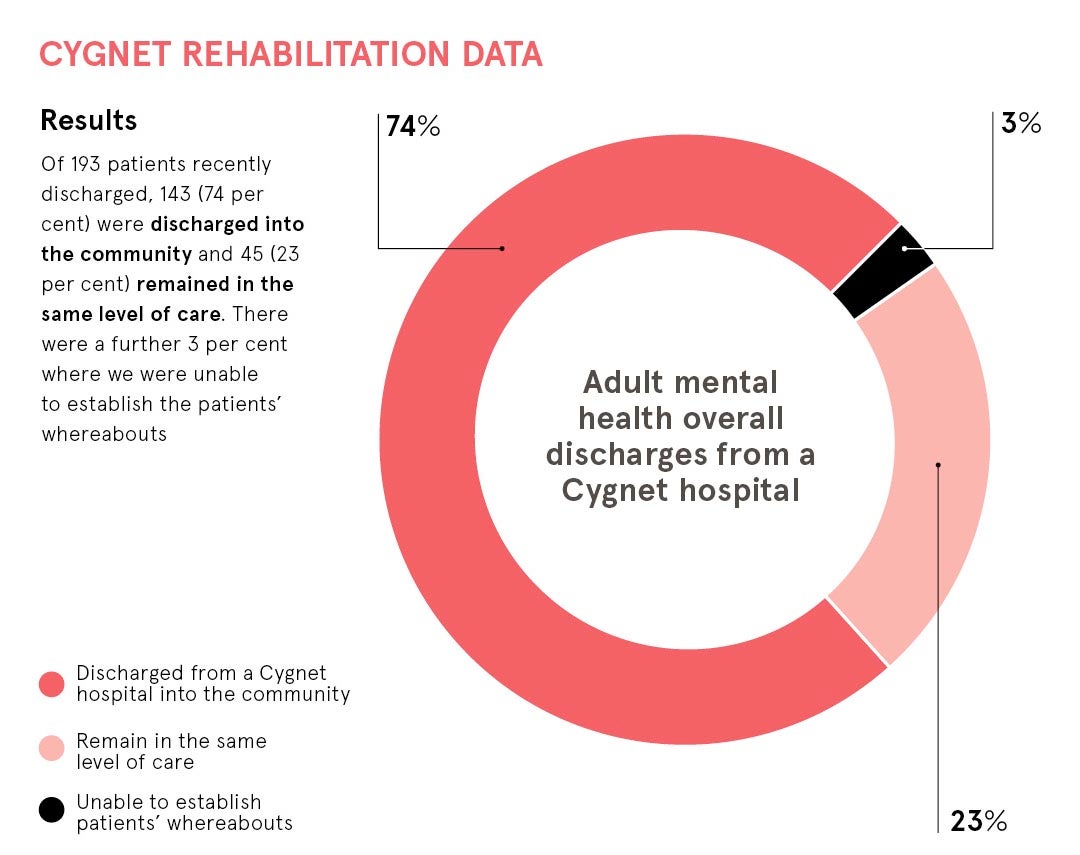
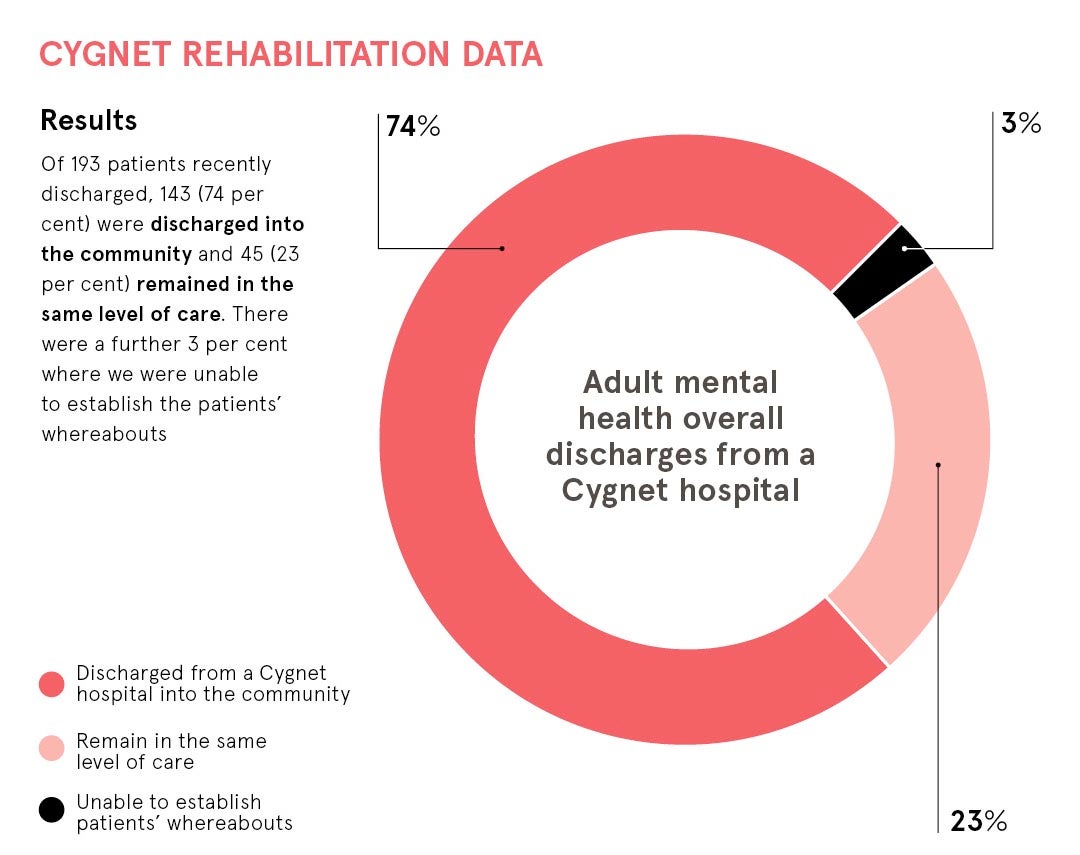
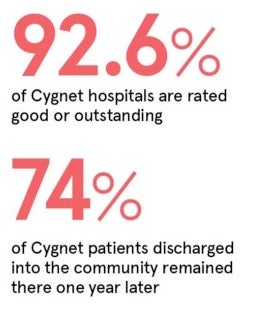
We have data from around 200 patients a year from high-support hospital and step-down rehabilitation services, covering different demographics, psychiatric profile and clinical outcomes. The data looked at patients who had been discharged into community settings, such as supported living, residential care or independent living, to see whether they had remained in the same or lower level of care, or whether they had relapsed and been readmitted to hospital. At least 74 per cent of our patients discharged into the community remained there one year later.
Nonetheless, there are standards that must be met across the industry to ensure successful outcomes like this, and we believe these need to be managed more appropriately and effectively to increase positive outcomes for all patients.
Private providers of healthcare should work in partnership with the NHS and the Care Quality Commission (CQC) to provide these services to the highest possible standards as it is our duty and privilege to provide care for these people who are some of the most vulnerable members of society. These facilities already welcome feedback from regulators and governing bodies, but more needs to be done to provide such services at a higher level and this is the responsibility of all parties involved.
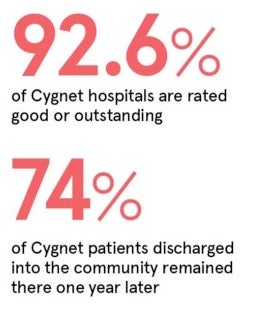 The industry needs to work together to improve its standards. The CQC’s The state of care in mental health services 2014 to 2017 report found that 76 per cent of independent services were rated as good or outstanding (72 per cent good and 4 per cent outstanding) and 23 per cent of independent services were rated as requiring improvement (three independent services were rated as inadequate). Cygnet is proud to offer the NHS a provision of high-quality hospitals and step-down facilities, 92.6 per cent of which are rated as good or outstanding.
The industry needs to work together to improve its standards. The CQC’s The state of care in mental health services 2014 to 2017 report found that 76 per cent of independent services were rated as good or outstanding (72 per cent good and 4 per cent outstanding) and 23 per cent of independent services were rated as requiring improvement (three independent services were rated as inadequate). Cygnet is proud to offer the NHS a provision of high-quality hospitals and step-down facilities, 92.6 per cent of which are rated as good or outstanding.
We believe that underperforming care facilities should be better monitored if they do not meet the requirements as laid out by the CQC
We believe that underperforming care facilities should be better monitored if they do not meet the requirements as laid out by the CQC. Although currently the CQC inspects mental health hospitals across five domains to ensure they are safe, clean, responsive, effective and well led, we believe an additional domain that focuses on the service user’s opinion of the care they received should also be incorporated. This would help to measure soft intelligence and ensure service users feel happy and well cared for in their care facility.
There should also be minimum standards of requirements to run a mental health facility. For example, facilities should be able to provide clear, on-site details of all on-duty staff, including full-time nurses, doctors, psychiatrists and therapists, and have them readily available. We also propose that initiatives such as the Accreditation for Inpatient Mental Health Services from the Royal College of Psychiatrists should form an active part of the review process, not just the CQC alone.
Moreover, we should never underestimate the importance of having an indicator of success. Relapse indicators should always be a factor when determining a patient’s outcomes and success in a high-support rehabilitation facility.
Providing effective high-support rehabilitation services is undoubtedly challenging. However, they are critical in trying to address the complex mental health care needs of a cohort of people, some of whom are among the most vulnerable. The most appropriate approach would appear to be service providers, the NHS and CQC working together to address the issues involved in effectively implementing these services. It offers the best opportunity of helping patients move through their recovery pathway, from specialised commissioned secure services through to non-secure rehabilitation services, with the eventual goal of returning back into the community.
Shortening this journey benefits not only the NHS and society as a whole, but most importantly the patient whose wellbeing is our ultimate priority.
For more information please visit cygnethealth.co.uk