Type-1 diabetes is not caused by lifestyle considerations. It is an auto-immune disease that destroys insulin-producing cells in the pancreas. When the body fails to produce insulin, glucose levels in the blood start to rise and the body cannot work properly.
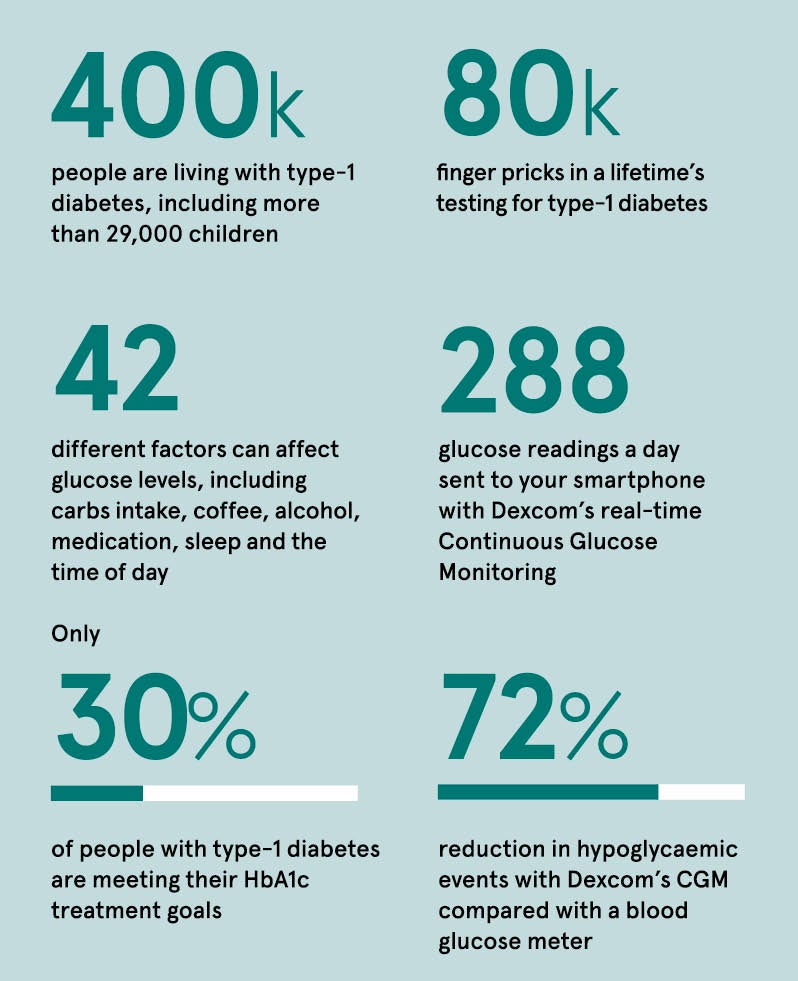
There is no cure for type-1 diabetes and the condition requires daily management. People with type 1 will have to prick their fingers on average seven times a day – more than 80,000 times over a lifetime – to measure their glucose level. Each test involves drawing blood from their fingertips using a lancet and a blood glucose meter. This is in addition to the multiple daily insulin injections.
Type-1 diabetes is a 24/7 condition that affects everything from concentration levels at work when your glucose level is high, to having to sit out sports lessons because your level is low. There are 42 factors that can affect blood glucose levels and keeping track can be draining emotionally. This is hardly surprising, given that regular hyper and hypoglycaemic events will lead to significant chronic complications affecting the eyes, kidneys, heart, brain, feet and nerves.
What is so alarming is that only 30 per cent of people with type-1 diabetes meet their blood glucose targets, according to the NHS National Diabetes Audit. This is why having a real-time continuous glucose monitoring system is so important.
Dexcom’s Continuous Glucose Monitoring (CGM) technology has revolutionised the daily routine of people with type-1 diabetes. It helps them reduce their HbA1c (average blood glucose/sugar levels) and can improve quality of life by removing the need for finger sticks,1 used to take blood samples. In five clinical trials, the use of Dexcom CGM technology has been proven to lower HbA1c, reduce the risk of hypoglycaemia, increase the time spent in range, and improve quality of life and wellbeing.
The technology is transforming day-to-day life for children and adults with type-1 diabetes, giving them confidence, for instance, to go for a solo run, sleep through the night without waking up to check their levels with a fingerstick, go to school, or enabling an elderly loved one to be at home alone.
People with diabetes can be more discreet in monitoring their condition at work or while socialising. It gives them freedom and peace of mind. With just a quick glance at their smartphone or watch,2 a Dexcom user is able to see their glucose levels, where they are heading (up or down) and how fast they are getting there.
By keeping patients well, the system is also helping the NHS, reducing the risk of hospital admissions. The NHS currently spends around £1 billion a year caring for patients with type-1 diabetes.
CGM is a diabetes management tool that measures glucose levels 24 hours a day using a small sensor inserted just under the skin. The device wirelessly transmits glucose readings every five minutes to a smartphone,2 smartwatch or receiver to provide users with real-time glucose readings. It also gives a warning when levels are too high or too low.
The Dexcom G6® works through Bluetooth technology built into the transmitter, and gives a complete viewing of glucose levels, trends and data. A small enzyme-based electro-chemical sensor measures glucose levels just underneath the skin. A transmitter fastened on top of the sensor then sends data to a compatible smart device2 with the Dexcom G6 app.
This enables people with type-1 diabetes to view their glucose trend and know when it’s high, low or within range. A Dexcom G6 receiver can also be acquired as an optional display device. It is fast, continuous and accurate.
Dexcom’s new Urgent Low Soon alert is designed to provide a 20-minute advance warning of an impending low, reducing the chance of a severe hypo even further. Users know they can trust their readings to make treatment decisions, such as eating for a low glucose level or dosing insulin for a high glucose level.
Loved ones can be kept in the loop as with Dexcom Share® up to five chosen followers can access the wearer’s glucose data.3 It is even possible to keep track of trends and estimated HbA1c with Dexcom CLARITY®, helping users and their medical team better manage their diabetes. The G6 is Dexcom’s slimmest device ever, 28 per cent thinner than the previous generation product, allowing users to wear closer-fitting shirts or dresses without unsightly bulges.

Natalie Balmain, from Manchester, is an entrepreneur with her own clothing business. When she was diagnosed with type-1 diabetes it changed so much about her lifestyle and friendships that she considers it the start of a second life.
She says Dexcom has made a profound difference. “Running my own business is incredibly demanding and I never have the same routine from day to day. So being able to customise my alerts depending on what I’m doing makes my life so much easier,” says Natalie.
There is no national funding for CGM through the NHS yet, although this may change as evidence grows of its benefits. At the moment people with type-1 diabetes are encouraged to talk to their healthcare professional about what they can do to access funding for a Dexcom system. Alternatively, they can self-fund. Dexcom offers a Subscribe and Save plan for full-time wear at £159 a month. A starter kit is also available for a one-month trial.
Karen Baxter, head of Dexcom UK and Ireland, says: “We believe our Dexcom G6 system will set new standards, both in terms of patient benefits and cost-efficiency for the NHS. We are working with healthcare professionals across the UK to make CGM more widely available through the NHS for patients with type-1 diabetes.”
For more information please visit www.dexcom.com
1 If your glucose alerts and readings do not match your symptoms or expectations, use a blood glucose meter to make diabetes treatment decisions
2 To view a list of compatible devices please visit www.dexcom.com/compatibility
3 Internet connectivity required for data sharing. Following requires the use of the Follow App. Followers should always confirm readings on the Dexcom G6® App or Receiver before making treatment decisions
Accuracy and clinical outcome studies: Wadwa RP, et al, Diabetes Technol Ther. 2018. Beck RW, et al. DIAMOND – JAMA 2017. Soupal J et al. COMISAIR, Diabetes Technol Ther. 2016. Heinemann L, et al. HypoDE, Lancet. 2018. Reddy M et al, iHart CGM Diabet Med, 2018. Lind M, et al. GOLD JAMA, 2017