In healthcare, as in most industries, software-based innovations are gradually replacing traditional hardware technology – unsurprisingly. Without a centralised integration system that allows for the effective gathering, storage, analysis and retrieval of information, devices like desktops, laptops, tablets and mobile phones have very limited potential in terms of improving patient care. Spending on hardware products that will be used as stand-alone devices is therefore also unlikely to generate significant returns on investment.
Health tech companies are now focusing on providing fully-integrated software platforms that deliver electronic observations, handover and task management solutions. Patient information is transmitted to a centralised storage system and is accessible by the entire care team, allowing for better medical decisions and increased work efficiency, thereby supporting staff in achieving high standards of quality and safety.
The electronic collection of vital signs at the bedside is revolutionary in itself. Dr Mark Simpson, consultant in emergency medicine and chief clinical information officer at Hull Royal Infirmary, explains: “It allows rapid identification by staff of changes in patient conditions and timely escalation of care through automatic calculation of early warning scores. For example, if there is a risk of infection based on the information being recorded, the infection control team is alerted, even before the individual staff member has considered the need to escalate.
New technology has the potential to prevent medical errors, improve transparency and increase the amount of direct care delivered
“However, these functions become much more powerful when combined with the two other key components of integrated systems, namely electronic task management and handover, allowing for effective ward-round and workforce planning, team structuring and feedback loops, all of which can thus become an actual part of the expected working practice.”
Dr Simpson adds: “Such an integrated system also reduces time-consuming events, such as chasing up medical staff on antiquated phone or bleep systems, and allows for centralised patient information to be available to multiple staff when needed, compared to one observation chart at the end of the bed. Or worse – not at the end of the bed.”
There are other benefits, too. Consultant anaesthetist, Dr Tim Bourne, chief medical information officer for University Hospitals of Leicester NHS Trust, notes that the new technology has the potential to prevent medical errors, improve transparency and increase the amount of direct care delivered. It is faster, more reliable and probably cheaper to maintain once in place and supported by a robust infrastructure, he adds.

Ultimately, more accurate data recording and analysis will allow for better decision-making by clinicians and improved quality of care, says Peter Greengross, medical director at The Learning Clinic, London. “Introducing the new system can also be an opportunity to re-examine working routines and, where appropriate, bring in best practice,” he says. “The only real physical requirement is a secure wireless network in the hospital, but these are increasingly common.”
Although there are up-front costs involved, the return on investment for using mobile solutions, such as electronic observations, for example, or task management for out-of-hours care, can be several times the initial investment and can be achieved within as little as a few months.
There is financial help available for hospitals that want to invest in technology. Several trusts have already been awarded shares of the £100-million Nursing Technology Fund and the £260-million Safer Hospitals, Safer Wards Fund, launched by NHS England to facilitate progress towards a paperless healthcare system. And, over the next two years, the Department of Health expects to distribute a further £35 million.
Trusts should also consider consulting previous hardware providers about the possibility of adapting and using part of their existing equipment, such as Dell desktops and laptops, for instance. Whenever possible, this can help make the most of investments already made, thereby reducing costs and waste.
Crucially, just as hospitals need to provide personalised care to their patients, health tech companies need to tailor products and services around the individual needs of their customers. An off-the-shelf approach, whereby the whole hospital platforms is merely replicated from elsewhere, will not succeed.
Dr Greengross of The Learning Clinic explains: “Every trust is different, so it is crucial that each one can select the functionality they want to add to the system. These can range from classic vital-signs recording to links to pathology and radiology systems. In addition, individual trusts may have specific procedures, such as escalation protocols, that need to be incorporated in the new system.”
Bespoke fully-integrated software-based solutions are opening up extraordinary new opportunities and possibilities, for healthcare professionals and decision-makers alike
Not only that, an IT system must be flexible enough to work efficiently across different hospitals within a trust. Off-the-shelf products simply don’t offer such flexibility, unlike bespoke solutions. The latter are also more likely to foster engagement, interest and motivation among staff. What’s more, according to Julia Ball, assistant chief nurse at University Hospitals of Leicester NHS Trust, they enable clinicians to retain ownership, which is all important to successfully implementing new technology. She adds: “Other key success factors include the availability of resources to support implementation, suitable mobile devices and the right infrastructure. Further, there is the need for a clear strategy, which must include plans for sustainability.”
As Dr Simpson of Hull Royal Infirmary notes: “The obvious, poor ability of paper records to optimise care is legend.”
Bespoke fully-integrated software-based solutions are opening up extraordinary new opportunities and possibilities, for healthcare professionals and decision-makers alike, to achieve high standards of quality and safety for patients, and truly revolutionise the future of healthcare.
CASE STUDY
From paper to cloud

Arguably one of the most exciting innovations in healthcare is the electronic recording of observations. The technology enables nurses to capture routine patient information on portable devices, such as computer tablets rather than a chart, reducing the risk of medical errors and missed care due to illegible, damaged or lost data.
Plus, the information is instantly available to all staff involved in the care of a patient, which allows nurses and doctors to identify quickly when there is the need for extra attention. Even more important, electronic observations allow for the automatic calculation of early warning scores, resulting in the prompt intervention of relevant medical staff, when a patient’s condition deteriorates.
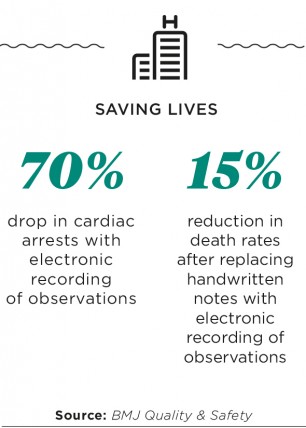
A study in BMJ Quality & Safety found that replacing traditional handwritten paper charts with electronic recording of observations reduced death rates by 15 per cent. The study, which was conducted in two large hospitals, also found a 95 per cent reduction in norovirus outbreaks and a 70 per cent drop in cardiac arrests. The average length of hospital stay was reduced by 17 per cent.
Importantly, an electronic observation system, and indeed the whole mobile integrated system deployed in a hospital or trust, requires a secure wireless network to function. In addition, experts recommend cloud technology for software provision and efficient, ubiquitous data storage, sharing and management.
According to a survey by HIMSS Analytics, in the United States, 83 per cent of healthcare providers have already embraced cloud technology and almost all plan to expand their cloud services. Why? Because, they say, cloud technology is relatively cheaper than buying and maintaining traditional on-site IT infrastructure, allows for faster speed of deployment and addresses the problem of having insufficient manpower or expertise for on-site alternatives.
In the UK, cloud technology was first used in 2011 to store NHS patient records online. Experts estimate that healthcare providers can realise a minimum 15 per cent saving on IT spending as a result of moving to this type of storage solution. A reason for this is that they have to pay only for the data space they use, which is considerably less expensive than building and running a data centre in every hospital.
Most importantly, cloud technology allows for patient information to be encrypted and, consequently, securely transmitted across networks. Healthcare professionals and patients alike can therefore access the information they need, when they need it and wherever they are. This improves considerably the patient’s journey from primary to secondary and tertiary care. Families can benefit from alert systems that can readily inform them if, for instance, a loved one has not taken their medicines. And high-quality care and services can be provided to all patients, including those in remote locations.

CASE STUDY
From paper to cloud

