Biodegradable stents, battery-free pacemakers, even assays in the lab which end the need for animal testing – advances in coronary medicine are coming thick and fast. And what’s exciting for cardiologists is how many developments are within grasp; these are not theories, but work in progress.
At a laboratory level, consider the new assay being produced by the Coventry University spin-out company InoCardia, founded by Helen Maddock, which has the potential to predict the drugs that will be a problem in terms of safety and efficacy, before they go into clinical trials.
Dr Maddock explains: “All drugs have to be tested for safety [phase 1] before efficacy [phase 2 and 3] trials, but testing the effect drugs have on the contractility of the heart has always been difficult. This is because it is very difficult to mimic the way the heart muscle works – it contracts and relaxes, but also fills and empties with blood at the same time; it’s a very dynamic muscle.
“So researchers have not been able to recreate that artificially very well and at best have been forced to use whole animals or less sensitive tests for research, which are not ideal and are not always able to predict effects on heart contractility at clinically relevant doses.”
Instead Dr Maddock’s team have developed what is known as a work-loop assay. It’s an in-vitro model, consisting of a muscle undergoing a “contract and relax” cycle while being stimulated via an electrical impulse. This way scientists can assess mechanical muscle performance to a new drug compound.
“Previously, drugs could get through initial lab tests and look safe, but prove problematic once they were being used in a proper phase-1 trial in humans. This isn’t just costly and wasteful, but potentially dangerous,” says Dr Maddock. She hopes the technique will be available for use by next January.
STENTS FOR HEART VALVES
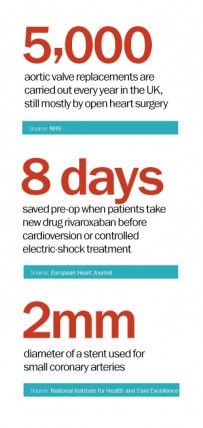
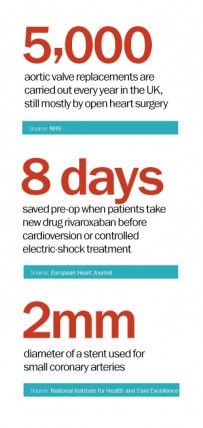
Over in the operating theatre, Vinnie Bapat, consultant cardiothoracic surgeon at Guy’s and St Thomas’ in London, is at the forefront of new techniques using stents to relieve blocked heart valves. “Traditionally, there were two ways of performing valve surgery: the gold standard of open heart surgery and more recently TAVI or transcatheter aortic valve implantation,” he says.
Now we have found a way to place a stent inside a previous stent to keep it open
TAVI is a much less invasive procedure. A stent or small tube is inserted into the damaged aortic valve via a catheter entering through the artery at the groin and is suitable for high-risk patients.
But both methods are being refined. In TAVI, stents with “skirts”, frilled edges which make the valve watertight and prevent potential dangerous leakage of blood in the wrong direction, are becoming available. New imaging techniques are improving surgical accuracy. Newly engineered stents are even flexible enough to be moved and repositioned if they are not perfectly sited first time. Some will be bioresorbable or biodegradable.
There is also stent-in-stent surgery, in which Mr Bapat’s team are world leaders. “Stents don’t last forever and the younger you are, the faster they wear out,” he explains. “Now we have found a way to place a stent inside a previous stent to keep it open.” He has helped build a teaching app for stent-in-stent surgery which is being downloaded worldwide.
In open heart surgery, new techniques are based around keyhole surgery. Mr Bapat continues: “At Guy’s, we are now carrying out 75 per cent of heart surgery in a minimal way, usually without the need to crack open the chest.” He expects it to be common practice throughout Britain within a few years, although open heart will always remain the gold standard.
One of the problems in heart surgery is ensuring patients are fit for procedures, a particular problem in atrial fibrillation (AF) cases, where cardioversion – a dose of electric current to the heart – aims to get the beat back into a normal rhythm.
Normal practice, says Oliver Segal, consultant cardiac electrophysiologist, at The Heart Hospital in London, is for patients to be on three weeks of successful, monitored warfarin anticoagulant therapy prior to the operation.
But warfarin is a notoriously tricky drug; it is effective, but not consistent, with poor patient compliance. “Some patients end up waiting months for their operation while we try to get three successive weeks’ results so that we can operate safely,” says Dr Segal.
DRUG TRIAL
Now results of a trial of a drug called rivaroxaban show that it could be an effective and well-tolerated alternative to warfarin, allowing for much more easily planned cardioversion. Dr Segal says: “It’s a great step forward in terms of managing AF as patients are getting cardioversion much faster on average than before.” The study found patients on rivaroxaban were then treated with cardioversion 22 days later as opposed to 30 days using warfarin.
Meanwhile, for patients with pacemakers, there is good news from the University of Bern, Switzerland, where scientists are turning the county’s clock-making expertise to smart use by designing a natural battery. “Pacemakers have two weak spots,” researcher Adrian Zurbuchen explains. “Leads are prone to fracture and the lifetime of batteries is limited.” He aims to use the motion of the heart to wind a spring, accumulating mechanical energy to power a pacemaker permanently.
The last area of innovation is monitoring, and here new telemedicine systems are ensuring data is collated and downloaded straight to cardiologists’ PCs, to ensure patients are treated more promptly and to spot potential acute incidents.
A recent meta-analysis in the Journal of Cardiopulmonary Rehabilitation and Prevention found emerging evidence that internet-based interventions, such as home monitoring, may reduce cardiovascular risk in cardiac patients and in populations with a heightened risk of CVD. It concludes that “such interventions may also represent an alternative method of providing CVD prevention strategies”.
STENTS FOR HEART VALVES