The internet has transformed the way we shop, with a visible impact on the high street as traditional retailers retrench. It may be less obvious, but the digital age has also had a profound impact on pharmacies. Millions of people now routinely buy medicines and wellbeing products over the internet, and seek health advice online.
Online shopping has shaken up a basic business model that had survived for more than a century with little change. Patients consulted their GP, who wrote a prescription for drugs or medicine. Patients then handed the prescription to their nearest pharmacist, who supplied the drugs prescribed by the GP. The pharmacist sought to supplement the modest income from providing the service by selling other, mostly health-related products to this steady flow of customers sent in their direction by the GP.
The internet has disrupted this model with online pharmacies giving consumers new choices and more control over how they manage their own health and wellbeing. At the same time, bricks-and-mortar pharmacies are having to rethink their role in the community, with many broadening their offering to customers as a response to the online challenge.
How online pharmacies cornered the market
Online pharmacies have been around for two decades, but it is in recent years that they have made real impact. Some 25 per cent of people in the UK say they are likely to use an online pharmacy in the future, according to a YouGov survey for the General Pharmaceutical Council earlier this year, and there are more than 350 registered UK online pharmacies. Pharmacy2U, the UK’s largest online pharmacy, has seen 300,000 patients use its NHS prescription service to have their medication delivered in the last 12 months, with a new facility in Leicestershire capable of dispensing 7.5 million items a month.
Established high street pharmacies, such as Boots and Lloyds, also now have a strong presence online, but customers are increasingly familiar with companies that only operate online, such as PillTime.
What drives this upsurge in demand for online pharmacies? It is important to note that it takes place against a background of an increase of more than 50 per cent in the number of items being prescribed by the NHS over the last decade. This is due mainly to the UK’s ageing population and because more people are living with a long-term condition.
How the NHS is learning from online pharmacies
Increasingly, people are using the internet to help to manage their health and wellbeing. In the United States, an estimated four out of five people go online before deciding to consult their family doctor or go to hospital and this trend is reflected in the UK. Doctors often advise against searching on Google for symptoms, but the NHS itself is encouraging more patients to use the internet when they engage with the health service, for online consultations or to book appointments. Babylon and similar digital GP services have gone mainstream.
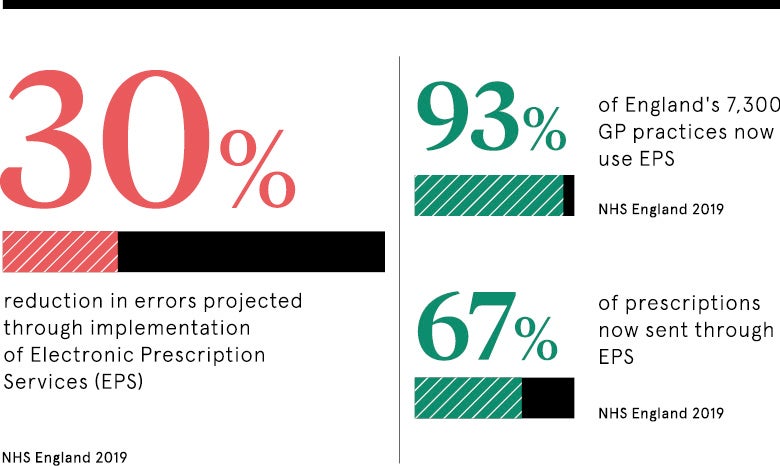
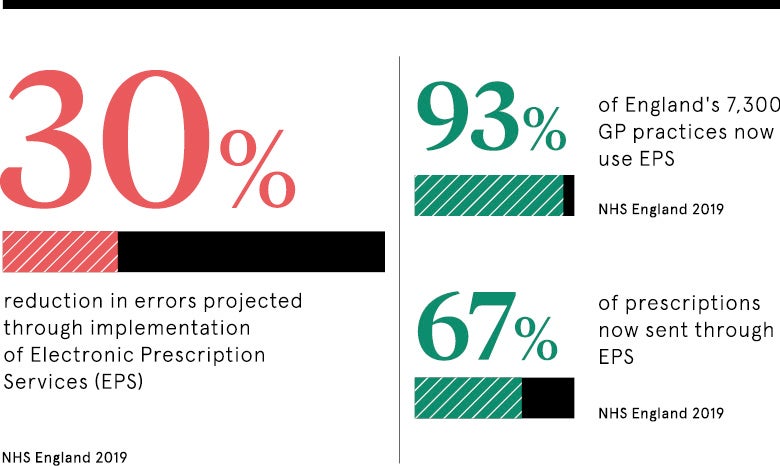
The NHS Electronic Prescription Service, which sends electronic prescriptions from GP surgeries to pharmacies, is increasingly popular and is likely to replace traditional paper prescriptions altogether. As well as saving costs for the NHS, it is helping to change the way patients think about their prescriptions, particularly those who have repeat prescriptions to treat long-term conditions. Patients can nominate an online pharmacy to dispense their prescribed medication, with the added benefit of having it delivered directly to their home.
As prescribing volumes increase online, bricks-and-mortar pharmacies are having to rethink their relationship with patients and their broader role in the NHS and social care. Hundreds of pharmacies have already closed, with many citing problems with new government funding arrangements. These have been implemented at a time when pharmacies face a number of pressure points.
The new role of the pharmacist in public healthcare
This changing landscape presents opportunities, as well as challenges. The NHS Long-Term Plan for England envisages an enhanced role for pharmacists at the heart of primary care networks alongside other health professionals, including GPs, nurses, physios, therapists and social care providers.
The NHS is putting some serious money behind the project, with a £4.5-billion cash injection designed to tempt GP practices to come together and set up neighbourhood teams staffed with pharmacists to review high-risk patients, reduce overmedication and improve the treatment of chronic diseases, such as asthma. The ambition is to move pharmacists away from dispensing drugs, and the associated administrative burden, to providing value-added patient services and care.
Keith Ridge, NHS England’s chief pharmaceutical officer, says: “From medication reviews for people on too many medicines to the reduction of inappropriate use of antibiotics, the skills of clinical pharmacists and pharmacy technicians working with patients, and the wider primary care team, will make a real difference to the communities we serve.”
Raising the profile of the community pharmacy
This is likely to see NHS England encourage more patients to use community pharmacies as their first port of call for non-urgent illnesses or health issues, with more pharmacists trained as independent prescribers. It will thus free up time for GPs to spend with patients reporting more complex needs.
Increasingly, community pharmacies will also be included in care plans when patients are discharged from hospital, helping to reduce readmissions. Pharmacies can then signpost patients to other services when required.
Health secretary Matt Hancock wants greater investment in IT to improve the integration of community pharmacies with health and care services. “Too often we reach to go to the GP when often our concerns can be solved within pharmacies,” he says. “I want us to be a country where more often the first port of call is to go and see the pharmacy.”
The clinical aspects of pharmacy are becoming more complex as new medicines enter the market, genomic medicine is starting to have an impact, and patients are becoming older, frailer and have more complex co-morbidities. Pharmacists are carrying out more patient-facing work than ever before and with this come changing requirements for training and demonstration of competence. Despite the challenges, it is an exciting future.
How online pharmacies cornered the market
How the NHS is learning from online pharmacies