Discovering you need medical help to get pregnant can be a devastating blow, but the postcode lottery for NHS-funded IVF treatment is adding to the stress and anxiety of many couples. At present, access to IVF in the UK doesn’t depend on your diagnosis or what would be best for you; it is entirely down to where you live.
People are borrowing money, crowdfunding, remortgaging homes or selling possessions to try to raise money for private treatment
The discrepancies in access to IVF treatment around the UK
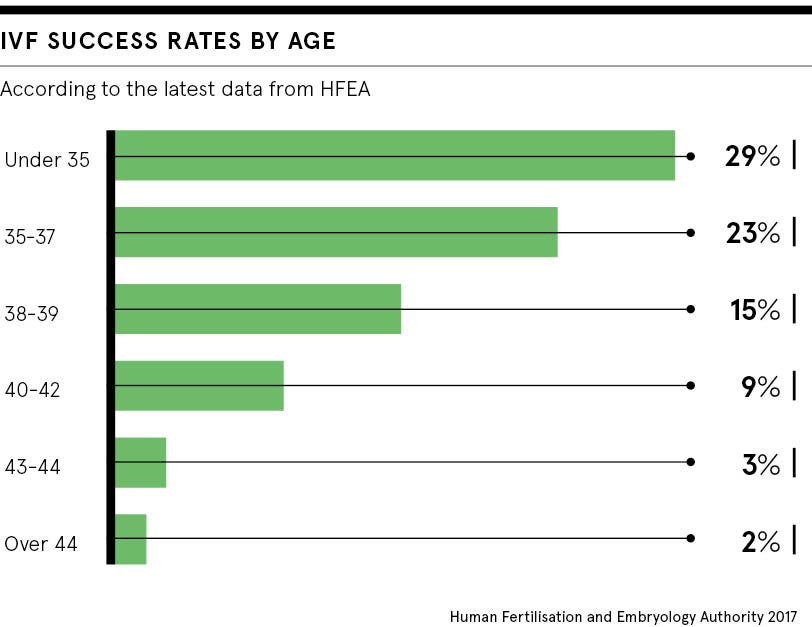
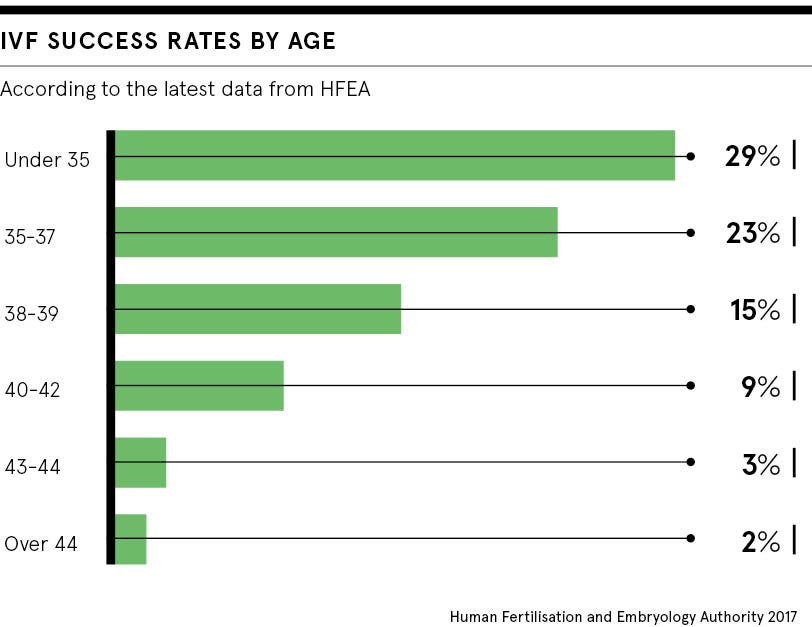
Back in 2013, the National Institute for Health and Care Excellence (NICE) produced guidance on the most cost-effective and clinically effective way of treating people with fertility problems. After careful analysis of all the available evidence, NICE concluded that eligible women of 39 and under should be offered three full cycles of IVF treatment and those aged 40 to 42, who met certain criteria, should be offered one full cycle.
In England, decisions about funding for IVF treatment are made by local clinical commissioning groups and recent figures suggest only 13 per cent are offering three full cycles. The majority provide a single cycle of IVF and some are not funding any treatment at all. The situation is different in the devolved nations where centralised funding decisions are made, but only Scotland is currently providing the three full cycles NICE recommends.
There are also some anomalies around the definition of a “full cycle” of IVF. Although NICE was clear that this should mean the fresh transfer, and freezing and future transfer of any additional embryos created, this has not been followed everywhere. Some have set their own definitions limiting the number of embryos that can be frozen and transferred.
Eligibility criteria can also reduce access to IVF treatment and you are unlikely to get NHS-funded IVF if you smoke, are overweight or underweight, or if you already have children. The latter usually includes children from previous relationships, regardless of how old they are or whether they live with you. Some areas have set their own age limits and others have additional restrictions around male age or weight.
Setting a benchmark for IVF costs on the NHS
IVF costs are often cited as the reason for restricting NHS services, but figures released by the campaign group Fertility Fairness to the Health Service Journal earlier this year showed that in some parts of the country local commissioners were paying twice as much for a single cycle of NHS IVF treatment as in other areas. NHS England is consulting on a benchmark price to help guide commissioners and this is likely to be less than some are paying at present.
Fertility specialist Professor Adam Balen, who chaired a group setting a benchmark price, recognises that for many people NHS funding is confusing. He’s made it one of the key issues at the Fertility Forum, an information day organised for fertility patients in London on March 30. “We realise many people find it hard to work out what they are entitled to,” says Professor Balen. “We put together our Fertility Forum to try to cut through the confusion when it comes to information about fertility and a session with campaign group Fertility Fairness will focus on explaining access to NHS-funded IVF treatment.”
What are the alternatives to IVF treatment on the NHS?
For those who find themselves denied access to treatment for whatever reason, the options are limited if you can’t afford private treatment. For younger women with good quality eggs, some clinics offer the option of egg-sharing, where a woman agrees to give some of her eggs to another patient who needs donor eggs, in return for a reduced treatment charge. Women considering this will need counselling beforehand. Some couples try to cut their IVF costs by opting for package schemes, which offer a number of cycles for a set price, or give money back if treatment does not work, but these schemes are not available for everyone.
If couples are going to fund their own treatment, they should look at the options available and make sure they have a clear idea of all the costs involved, rather than the headline prices on clinic websites. Setting a budget of what is affordable may help, along with comparing prices, as paying more for IVF does not always mean a better service. Many clinics offer an array of additional treatments, which can increase costs considerably.
Some couples investigate IVF treatment options abroad to try to cut costs. This can appear cheaper, but there is additional expense travelling to the clinic and paying for somewhere to stay. Couples may also have to pay for scans and tests they need in the UK during treatment.
Government need to find ways to help ease the heartache
Last month at Downing Street, Fertility Network UK chief executive Aileen Feeney presented a petition signed by more than 100,000 people calling for an end to the postcode lottery for IVF treatment. It was part of the patient charity’s Scream 4 IVF campaign aimed at halting the inequality of IVF funding.
“At Fertility Network UK, we see the heartache behind funding cuts,” says Ms Feeney. “We see people borrowing money from friends and family, crowdfunding, remortgaging their homes or selling possessions to try to raise money to pay for private treatment. That’s why we need fair access for everyone.”
Fertility Network UK also sees many people who have to say goodbye to their dream of becoming parents because they cannot afford to pay. Living with fertility problems is tough. It is often hard to talk about, and many couples experience depression and isolation. Findings from a Fertility Network UK survey suggest that a shocking 42 per cent have experienced suicidal feelings.
Every aspect of day-to-day life can be affected by fertility problems and struggling to access treatment adds a significant burden. IVF treatment cannot provide solutions for everyone, but there is little more distressing than finding you are unable to get the medical treatment which offers hope.
The discrepancies in access to IVF treatment around the UK
Setting a benchmark for IVF costs on the NHS