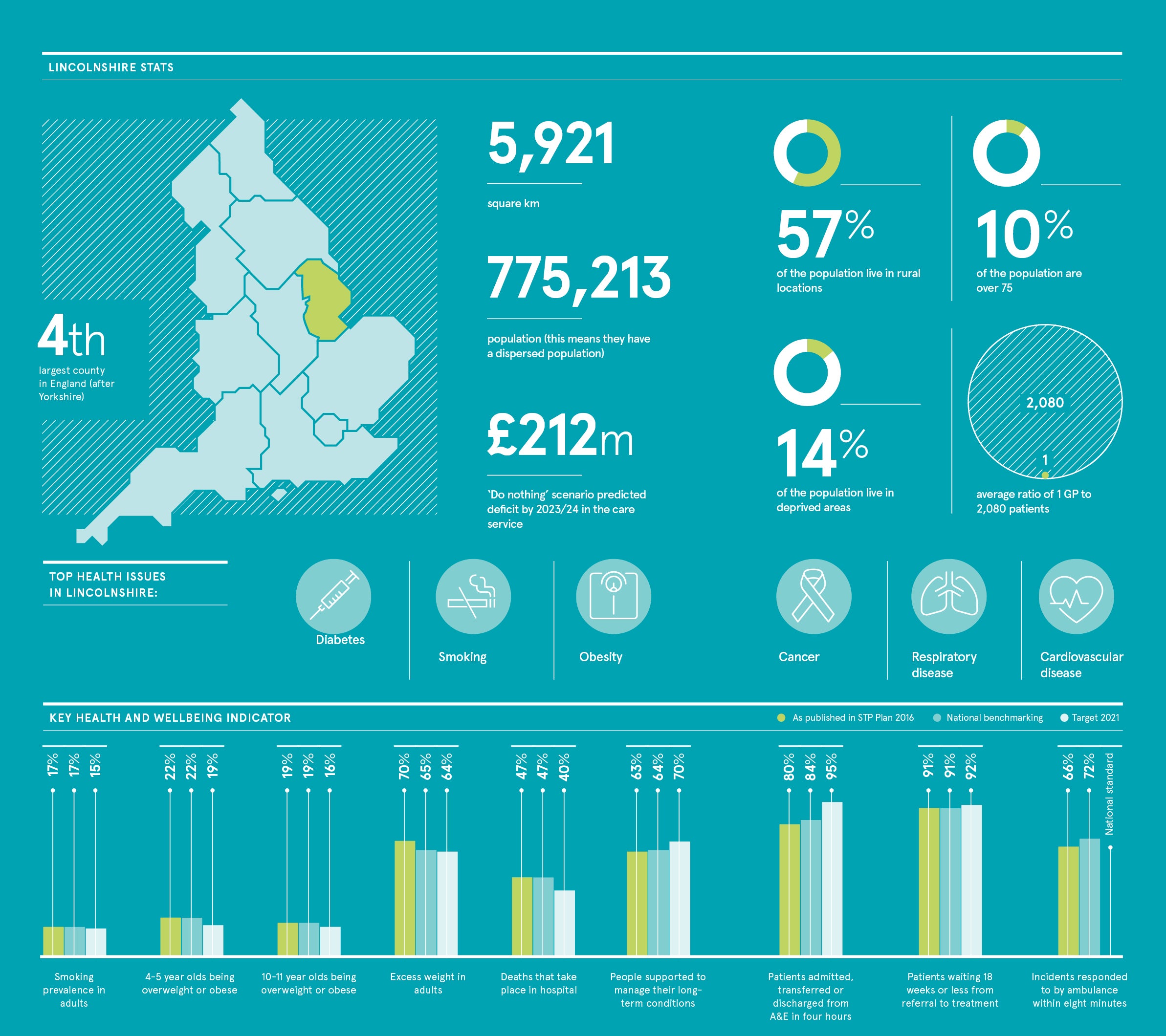
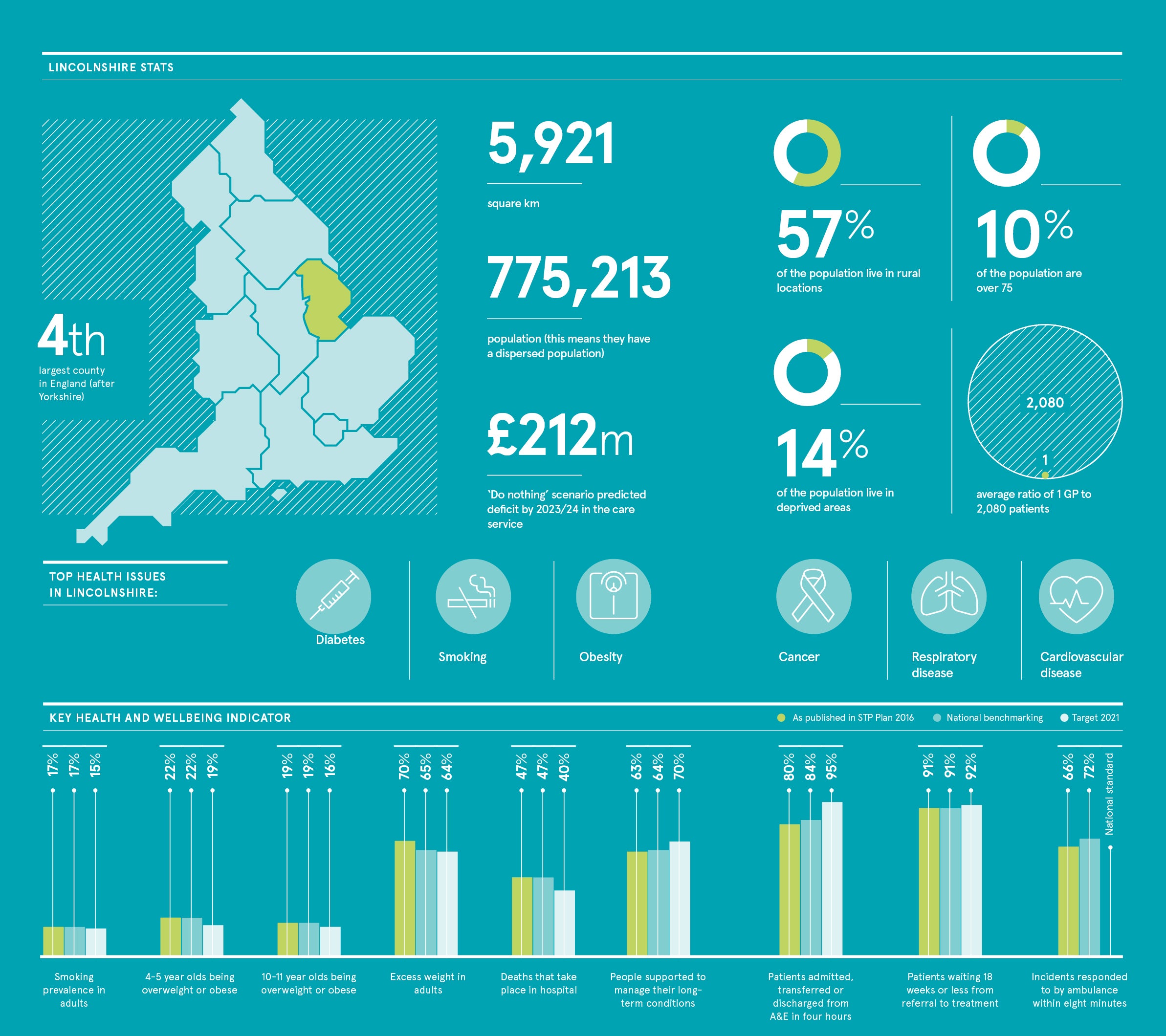
Many of the challenges facing the NHS are writ large in Lincolnshire. The fourth-largest county in England, more than half its population live in rural locations and, with one in ten residents over the age of 70, it has a disproportionately large elderly population. Alongside this, it is having to work harder than ever to make every penny count.
To meet these challenges, in 2013 Lincolnshire’s healthcare partner organisations undertook a major review aimed at transforming its health and social care services, and exploring how it could work more effectively with the third sector. Its goal was also to move healthcare out of hospitals, closer to patients’ homes wherever possible.
“We talked to colleagues across the care service, patients and others to ask the simple question, ‘If we want to deliver care differently, bring care closer to people at home and to bring about more integrated working, what do we need to be able to do?’” explains Liz Jones, project manager at NHS Lincolnshire Sustainability and Transformation Partnership (STP).
“When we asked this question the biggest issue that came up was the inability to access pertinent information across different organisations, GP practices, hospitals, community and social care providers. By making this change to care delivery it means that patients won’t have to repeat their story every time and clinicians would have faster access to information to make faster decisions which ultimately means better care.”
In an ideal world the answer would have been to create a brand-new, single overarching patient information system available to all health and care professionals, including its acute trust, community hospital, mental health trust, ambulance trust, 85 GP practices, and social and community care services. However, cost, time and continuity of care makes this option prohibitive.
Patients are already noticing that clinicians are better informed and they’re not having to repeat information to each person they see
Instead Lincolnshire’s healthcare leaders looked at how to bring together the myriad existing systems into a unified patient record, now live and called Care Portal. This meant having to focus on overcoming an increasingly significant challenge facing the health service: interoperability.
The technology powering the Care Portal is provided by InterSystems, a global leader in information technology platforms across health, business and government. InterSystems had already been providing services in Lincolnshire and across the NHS for some time, so the company knows the health and care situation well.
Already access to Care Portal means clinicians from the major healthcare organisations who are seeing a patient can login to the single, secure portal and view the relevant history from any of the connected systems. This is particularly important as patients could potentially have a range of conditions such as diabetes, mobility problems or mild dementia.
A community nurse can do the same before visiting a patient and if that patient is admitted to A&E or needs help out of hours, the doctors and nurses supporting them are no longer forced to rely on simply asking them questions and hoping they get the right answers.
“The more information clinicians have, the better decisions they can make,” says Yossi Cohen, physician executive at InterSystems. “They can also make them faster. Patients, meanwhile, are already noticing that clinicians are better informed and they’re not having to repeat information to each person they see. They spend less time waiting, wondering what’s happening with their treatments.”
“Because the information is not transferred in to one central database, and instead queries organisational information repositories, it ticks a lot of the information governance boxes. The system also supports Role Based Access Control (RBAC) and requires users to claim a relationship with the patient, before they can see any information”, explains David Smith, IT programme lead at NHS Lincolnshire STP.
The system is dynamically building up a record of which healthcare professional is involved with a particular patient. This is important because whereas historically a community nurse might, for instance, find themselves needing to speak to the relevant hospital doctor or care worker, but would not have any idea of the identity, let alone the contact details, of these people, now they can get this vital information quickly and easily by looking at who has logged in to the system to view the patient’s data.
The system goes further by alerting the care team. For instance, community nurses can be notified immediately if a patient has been admitted to hospital, avoiding wasted home visits. These can then be automatically rescheduled once a patient is discharged as well as discharge letters and outpatient records being accessible electronically and shared in real time.
Needless to say, the system is constantly being updated and tweaked in response to feedback from its more than 5,000 users, a figure that has risen tenfold since its introduction last autumn. “We found we were getting a lot of information that was repeated because a patient was being seen by two or three clinicians and we had to ‘declutter’ the portal so information was only given once,” says Ms Jones, project manager at NHS Lincolnshire STP.
The scope and capability of Lincolnshire’s groundbreaking Care Portal system is constantly growing. A connection with child protection records will match up hospital visits across the county and over borders to flag up instances where these visits are worryingly frequent.
Another innovation will see the introduction of a patient portal that allows patients to gain more access. This is starting with maternity services, where patients will be able to self-refer using a smart form, Interoperability: the vital ingredient speeding up access to antenatal care. Meanwhile, wearable technology will enable health and social care professionals to share essential information about how a diabetes or cardiac rehab patient is recovering, providing alerts immediately should a problem arise.
“The fact that so many clinicians are using the Care Portal system shows how much it’s needed and how keen staff are to engage with it,” Mr Smith concludes. “We have a long list of other systems that people want to have connected now they’re already seeing the benefits of this kind of interoperability.”
For more information please visit InterSystems.com/uk/health
Interoperability: the vital ingredient
Healthcare providers are increasingly realising the vital importance and benefits of enabling patient care systems to “speak” to one another
You can have all the sophisticated technology and comprehensive datapoints imaginable, alongside trained and engaged healthcare professionals, but if these constituent parts can’t “talk” to each other they can’t help patients.
It’s little wonder then that interoperability has become such a priority for the health service. According to the 2018 NHS IT Leadership Survey, 82 per cent of those asked said interoperability that enabled systems and staff to share patient information was their top priority, up from 51 per cent in 2017.
It’s clear that one of the keys to better interoperability is standardisation. The NHS centrally and locally, along with its suppliers, needs to work together to deliver agreed standards so local services can be more agile and respond to patients’ needs more quickly and appropriately.
We need to recognise shortcomings quickly and work in an agile way to meet clinical needs swiftly and to be responsive
According to David Hancock, healthcare executive adviser at InterSystems: “Standards across organisations are important because without them, all you’ll only be able to do is send documents to clinicians that end up rarely read or viewed. Using standards allows information to be delivered in far more usable and convenient ways.”
However ingenious the technology, digital transformation of the kind that is so successful in Lincolnshire, relies on executing a clear vision. This means putting the groundwork in early to engage all the contributing people and organisations, together making appropriate adjustments along the journey.
“We need to recognise shortcomings quickly and work in an agile way to meet clinical needs swiftly and to be responsive,” says Yossi Cohen, physician executive at InterSystems. “Most importantly, we also need to ensure that clinicians can easily adopt it and reap the benefits. This means involving frontline care providers from the beginning and throughout the implementation.”
It’s fair to say that many health and care providers will be open to technology that makes their lives easier and enables them to deliver better healthcare more quickly. Unfortunately, they can often lack the time and the patience to learn to use new systems, says Mr Hancock.
To win over hearts and minds, IT and digital transformation leaders need to work with the willing by identifying champions, those who can spread the word and demonstrate the benefits from their own experience.
IT leaders also need to listen to staff, allowing them to contribute their own ideas. Dr Cohen concludes: “Digital road maps need to be clinically driven so clinicians buy into the technology and their patients can benefit from the exciting new opportunities it offers.”
For more information please visit InterSystems.com/uk/health