Cancer treatment has come a long way since mustard gas was first tried in the 1940s to treat lymphoma patients. Better treatments have emerged that have changed the outlook for those with the disease. Mortality rates have significantly decreased and are projected to fall a further 15 per cent between 2014 and 2035, according to Cancer Research UK.
But although modern-day hospital-administered systemic anti-cancer therapy (SACT) is a far cry from the primitive therapeutic agents spawned by deadly weapons, it can still be a stressful, time-consuming and exhausting experience for patients and their families.
James Casey from Huddersfield was devastated when, four years ago, he received a diagnosis of peritoneal mesothelioma, a form of cancer caused by asbestos, which affects the lining of the abdomen. As there are few doctors who specialise in this condition, Mr Casey was placed under the care of a consultant, based more than 100 miles away in Leicester. For greater comfort and convenience, the consultant recommended treatment outside hospital.
You cannot underestimate the additional convenience treatment in the home can bring to the patient
“I was so poorly in the early days after diagnosis that I might have refused to go to the hospital because I was feeling so ill. It made a massive difference for nurses to come to my home and carry out the treatment. And it meant my friends and family didn’t have to take time out to visit me in hospital,” recalls Mr Casey, whose clinical home care is arranged by Healthcare at Home, the UK’s leading provider of clinical services given outside of hospital. “Without a doubt, it is a fabulous option for patients.”
“The truth is that hospitals can be scary places sometimes,” says Professor Sir Jonathan Asbridge, Healthcare at Home’s chief clinical officer. Around 6,000 patients are treated for cancer at any one time by the company and 450 SACT regimens are supported.
Many of the most commonly diagnosed cancers have a ten-year survival rate of 50 per cent or more, according to Cancer Research UK, but the treatment journey can still induce complex emotions for the patient, including a feeling of losing control of their life.
“One breast cancer patient in her late-30s recently told me: ‘I haven’t missed a day of being here for when my kids come home from school’,” says Sir Jonathan. “She stays at home rather than driving 60 miles to have SACT in the hospital.” 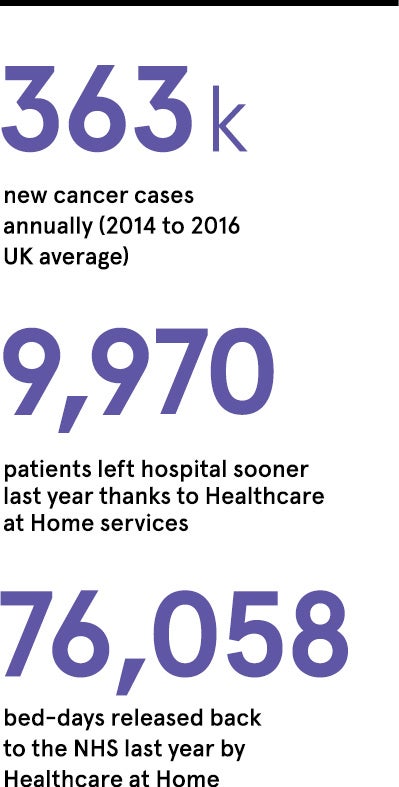
At-home cancer treatment needs to be as unobtrusive as possible, he explains. It should fit around the person’s life.
“You cannot underestimate the additional convenience treatment in the home can bring to the patient. Having SACT in a hospital involves travel, finding a parking space and, when you arrive, having bloods taken and waiting for the medication to be compounded. Often this can lead to a patient attending a hospital for the whole day for treatment that may only take an hour or two,” says Sir Jonathan.
But Healthcare at Home clinicians visit the patient two days before the medication is given to carry out the necessary blood tests and patient assessments, and conduct a clinical pre-assessment. This ensures on the day of medication the patient isn’t waiting around. “We bring the cancer therapy straight to you. All the patient does is have the treatment for that period of time and then they can get on with their life,” he says.
Sir Jonathan, who is also president of the European Society for Person-Centred Healthcare, says patient choice must be the future of clinical care. There’s a growing body of evidence supporting clinical home care for various medical conditions.
One study found care at home was associated with a 38 per cent reduction in mortality at six months compared with hospital treatment. And home treatment may also reduce the risk of a cancer patient with a compromised immune system contracting an infection.
As well as good clinical outcomes, there are financial benefits for medical insurers and private patients who elect to self-pay, as some cancer medications are VAT exempt when administered at home.
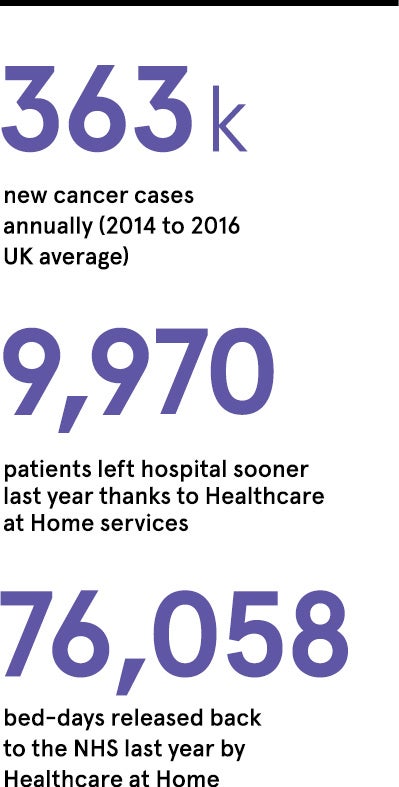
Some of Healthcare at Home’s other services, such as infusion care, provide advantages for the NHS too, as by enabling discharge as soon as patients are medically fit, this can free up beds. Clinical home care may also reduce unplanned hospital admissions and waiting times.
The benefits for hospitals and patients sound impressive, but can SACT at home really be safe for everyone? Sir Jonathan cautions that a thorough risk assessment must be undertaken first. However, he points out that many hospital-type services can be safely given at home with patients remaining under the care of the referring consultant at all times.
For NHS patients, guidance is always sought from the local hospital to ensure the treatment provided is consistent with their clinical protocols. All Healthcare at Home’s specialist cancer nurses are trained to either degree or masters level, or hold an NHS-accredited chemotherapy qualification. They all undergo annual SACT accreditation to ensure their knowledge and skills are up to standard. And all patients have 24/7 access to a team of cancer clinical nurse specialists who support them and their families throughout the pathway.
Healthcare at Home has recently invested in a major digitalisation programme which it hopes will put even more control in the hands of patients, so they can arrange appointments and track medication deliveries online. Sir Jonathan is optimistic about the future of cancer treatment and believes combining research breakthroughs and patient-centred care could make a huge difference to people’s lives, “enabling them to have their best day, every day”, he says.
For more information please visit www.hah.co.uk/cancer