It is widely accepted that early diagnosis saves lives and significantly reduces the financial burden of disease, wherever you are in the world.
This is a key priority for the NHS, social care and the government, but with a health system historically focused on treatment, how can the NHS realise the real potential of early detection?
The Japanese health system has taken health services out of hospitals and into communities, and has made regular health checks the foundation of everything it does.
Annual health checks empower patients to monitor their own health routinely by offering preventative services, including diagnostic point-of-care testing and screening, in community health centres and mobile facilities.
As we strive to continue improving patient outcomes in both countries, Fujifilm believes this diagnostic- and community-led culture offers important lessons for the NHS to consider.
How community-centric healthcare works in Japan
Japan’s move towards a community-based integrated care system was in part inspired by the small, rural town of Mitsugi. In 1984, the town opened a local health management centre, and in 1997 the community care department of the municipal government was moved to this centre, so public health nurses could provide preventive care such as health check-ups directly within the local community.
Since then, community-centric healthcare practices have spread across Japan, empowering local health centres and making diagnostic services more accessible to patients.
The Japanese government has embraced these practices; municipal governments now provide health checks for their residents, including several which are legally required, at the local level.
According to the Organisation for Economic Co-operation and Development (OECD), Japan now has arguably the most extensive range of health check-ups and screenings of all OECD countries.
There is clearly an opportunity for the NHS to learn from the Japanese system and challenge the status quo
While the exact nature of annual health checks varies in different Japanese localities, a typical check entails a low-dose chest x-ray, urine test, girth, height and weight measurements, blood pressure check and various blood tests.
Attending annual health checks at local screening centres or in mobile vans has become an ingrained feature of Japanese society and helps to keep patients out of hospital.
The UK can learn from this model, which truly prioritises early diagnosis, delivering a culture of local-level prevention that reduces unnecessary hospital admissions and saves resources; a key feature of the NHS Long-Term Plan.
Catching cancer early: how regular screenings can save lives
Regular screening attendance greatly improves the opportunity to detect early signs of disease, which significantly impacts patient outcomes. For example, Japan has one of the highest global rates of stomach cancer; as a result, endoscopies are included as part of patients’ standard annual health checks from the age of 40.
Japan’s ministry of health, labour and welfare also recommends that breast cancer screening takes place every two years for women aged 40 and over, a lower starting age than many comparator countries.
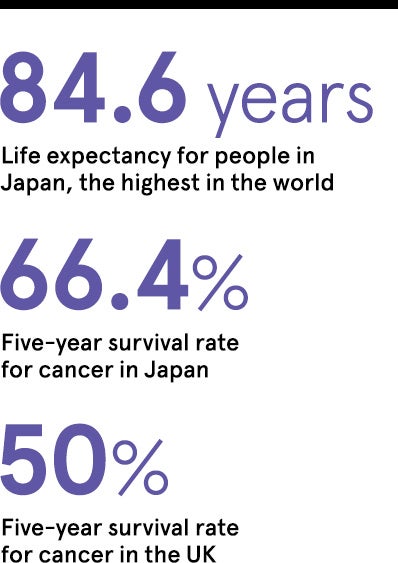
Early detection has helped Japan achieve the third-lowest mortality rate for breast cancer among OECD countries. More broadly, the five-year survival rate for cancer in Japan is 66.4 per cent.
At the other end of the spectrum, the UK is among the top-ten OECD countries with the highest breast cancer mortality rates, and the UK’s five-year survival rate for cancer overall sits at just 50 per cent.
Japan’s approach to prevention and diagnosis means that cancer screening is an engrained part of society. By contrast, the UK’s system sees below-target levels of screening uptake, including in breast, cervical and bowel cancer.
As Sir Mike Richards highlighted in his recent review into adult cancer screening in England, a central reason for low uptake of screening is the accessibility and ease of screening appointments.
There is clearly an opportunity for the NHS to learn from the Japanese system and challenge the status quo of hospital-centric services.
Opening the door to mobile screening technologies
At Fujifilm, we know that a successful community-based prevention model must be supported by the right technology. We will never stop developing innovations to help health services diagnose disease earlier, applying our heritage and expertise from the world of photography to create new diagnostic technologies for cancer screening to blood chemistry analysers that are more targeted at screening services which can be taken closer to the community. 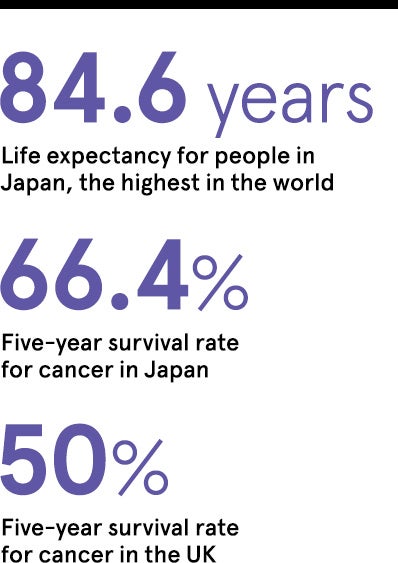
Point-of-care technology has become an essential tool in Japan’s community screening model and has the potential to transform the ability of local healthcare services in the UK to ease capacity for secondary providers and deliver greater preventative care.
Our mobile x-ray technology, such as the FDR nano with integrated artificial intelligence (AI), can also support the NHS to deliver faster, more efficient cancer screening in local communities or hard-to-reach areas. Weighing only 90kg, the FDR nano is an exciting example of a highly mobile lung cancer screening system that combines high-image quality, low-dose x-ray, and real-life triage and high levels of diagnostic accuracy through integration with AI technology.
Utilising these types of existing technologies in a community setting has the potential for the NHS to ease pressures on its workforce and save money, without sacrificing diagnostic accuracy.
The Japanese system has embraced innovative mobile and point-of-care technology to deliver a unique level of local preventative care. To challenge our hospital-centric status quo, the NHS should learn from this approach and empower local providers to deliver rapid diagnosis and support prevention.
Future of early detection
Adopting features of the Japanese model of community health could greatly improve early diagnosis and outcomes for patients in the UK. Moving towards a system which places greater emphasis on prevention, utilises point-of-care technologies and mobile screening services, and delivers truly local services, can all contribute to speeding up detection of disease and save NHS resources.
As the NHS looks for ways to boost the prevention agenda and deliver earlier diagnosis, it would do well to consider the Japanese way of working, for the benefit of all patients.
For more information please visit fujifilm.com/neverstop
How community-centric healthcare works in Japan
Catching cancer early: how regular screenings can save lives
Opening the door to mobile screening technologies