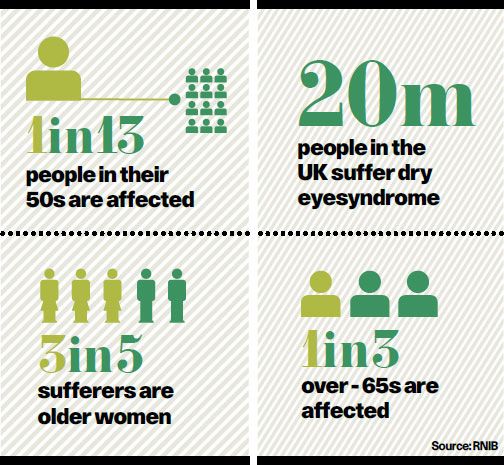
If your eyes get red or sore you might be one of 20 million people across the UK with dry eye syndrome. Often called dry eye, the condition can be uncomfortable, but is not usually serious.
Around one in 13 people in their 50s experience it, rising to one in three of over-65s because we produce fewer tears in old age. Older women comprise 60 per cent of sufferers, usually due to hormonal changes.
Precipitating factors include central heating, wind, smoke, medical side effects, contact lenses or infrequent blinking.
About 40 per cent of people get dry eye 30 minutes after prolonged close work – it’s an unrecognised epidemic
Dr Sandip Doshi, senior optometrist at the Eyecare Centre, Hove, says: “Tears play an essential role in how our eyes work, contributing towards good vision. We’ve all experienced blurry vision when crying, but similar problems can occur due to external factors causing dry eye.”
C.T. Pillai, founder and medical director of London-based laser eye surgery clinic AVC, says dry eye is characterised by disturbance in the tears covering the transparent eye-front or the cornea.
“When we blink, a thin tear layer covers the cornea which keeps eyes moist. Dry eye can occur when there is a dysfunction in the meibomiam glands producing the tears. Simple steps such as using humidifiers to restore room moisture or decreasing air-conditioning fan speeds can sometimes help.”
Research indicates dry eye may be reduced by consuming foods rich in Omega 3 or through innovative treatments, such as professionally designed, warm eye poultices.
Consultant ophthalmic surgeon at West Yorkshire’s Calderdale Royal Hospital Teifi James explains the two dry eye types. “Evaporative dry eye affects up to 40 per cent of the UK population, but Sjogrens syndrome, caused by tear gland failure, is rare. If you can produce tears, you haven’t got Sjogrens.
“If the lacrimal function unit, which produces tears, breaks down, then eyes don’t make enough tears or the tears evaporate too quickly, which causes dry eye. About 40 per cent of people get dry eye 30 minutes after prolonged close work – it’s an unrecognised epidemic.” Mr James advises warm compresses and regular computer breaks.
One dry eye complication is conjunctivitis – inflammation of the cell-layer inside the eyelids – which causes painful, sticky eyes. It usually improves without treatment, but lubricant eye drops can be purchased at pharmacies.
Common diagnostic method, the tear break-up time test, demonstrates how quickly the tear film breaks up after blinking; the shorter the time, the more severe the dry eye. In the Rose Bengal test, the optometrist observes how long tears take to evaporate, while the Schirmer test is used in severe cases.
Ian Grierson, ophthalmology professor at Liverpool University, comments: “The main issue with chronic dry eye condition is that, if not addressed, it can create symptoms from itching and inflammation to pain and visual disturbance.”
He acknowledges mineral supplements may reduce symptoms by encouraging the eyes’ natural hydration.
Geoffrey Ballantine, of Edinburgh optometrists Ballantine Goldie, says treatment varies. “If dryness results from working environment, we may discuss blinking exercises or eye-drops,” he says. “With blocked secreting glands, hot compresses or eyelid care might help. Dry eye management involves a custom-made individual approach.”
ALLERGIES
No hay fever, no cry
Spring has arrived bringing with it hay fever or seasonal allergic rhinitis, a reaction to pollen which irritates the lungs and nose, as well as the eyes, causing soreness and itching.
Optometrist Tracy Goldie, of Ballantine Goldie Optometrists in Edinburgh, says: “Signs of ocular hay fever also include inflammation of the conjunctiva – the thin membrane covering the eyelid’s inner surface and the whites of the eye.”
She adds: “If symptoms are just watery and itchy eyes, antihistamine eye drops from chemists or on prescription bring rapid relief of ocular inflammations.”
If exposure to pollen is unavoidable, contact lenses and/or sunglasses provide eye-protecting barriers to minimise symptoms.
Simon Madge, consultant ophthalmologist at Nuffield Health Hereford Hospital, says: “As a lifelong hay fever sufferer myself I understand only too well the eye discomfort it brings. Lubricant eye drops – artificial tears – available over the counter represent the first treatment stage.
“If these don’t completely relieve symptoms, sufferers can take eye drops containing sodium cromoglycate, which stabilises the mast cells causing hay fever. These take time to work so can be started before the hay-fever season.”
Anecdotal evidence suggests limiting wheat and dairy intake can reduce symptoms. Hay fever isn’t usually serious but, if symptoms persist, see an optometrist.
